Definition and Symptoms of Plantar Fasciitis

Plantar fasciitis is a common foot ailment characterized by inflammation of the plantar fascia, a thick band of tissue that connects the heel bone to the toes. The condition typically results from repetitive strain or excessive stress on the feet, causing tiny tears in the ligament. Individuals with plantar fasciitis often experience a stabbing pain near the heel, especially with the first steps in the morning. This discomfort may gradually subside during the day, only to resurface after prolonged periods of standing or intense physical activity. The pain tends to be more pronounced after sitting for an extended duration and can impact daily activities, affecting the overall quality of life. Understanding the definition and recognizing the symptoms of plantar fasciitis is essential for timely intervention and management. Plantar fasciitis can cause severe pain and discomfort. If you have developed this condition, it is strongly suggested that you are under the care of a podiatrist who can guide you toward the correct treatment method.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Joshua David Scoll from Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Recurrent Ankle Sprains

Recurrent ankle sprains pose a persistent challenge, impacting both daily activities and long-term joint health. When the ligaments surrounding the ankle undergo repeated stress or fail to heal properly after an initial sprain, individuals become susceptible to recurrent injuries. The telltale signs include swelling, pain, and instability, often accompanied by a popping or tearing sensation. Factors contributing to this cycle of sprains range from inadequate rehabilitation after the initial injury to anatomical predispositions and muscle imbalances. Individuals experiencing recurrent ankle sprains may find their range of motion compromised, affecting mobility and overall foot function. If you have sprained your ankle for the first time, or are experiencing recurrent ankle sprains. It is suggested that you are under the care of a podiatrist.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Dr. Joshua David Scoll from Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.
Adult Flat Feet and Their Underlying Causes

Adult flat feet, a condition where the arches of the feet collapse, can be attributed to a multitude of factors, each contributing to the intricate landscape of this common ailment. One primary cause is weakened or overstretched tendons, often stemming from prolonged wear and tear or injury. Age-related changes to tendons and ligaments can also impact foot structure, leading to the development of flat feet. Genetic predispositions often play a role, as individuals with a family history of flat feet may be more susceptible. Certain medical conditions, such as arthritis, diabetes, or obesity, contribute to altered foot mechanics and increased stress on the arches. Pregnancy is another factor, with hormonal changes and increased weight-bearing influencing foot structure. Wearing unsupportive footwear, especially during critical developmental stages, can contribute to the prevalence of adult flat feet. If you have flat feet, it is suggested that you visit a podiatrist who can offer you relief techniques, which may include custom-made orthotics.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Joshua David Scoll from Pennsylvania. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
What Is a Diabetic Foot Ulcer?
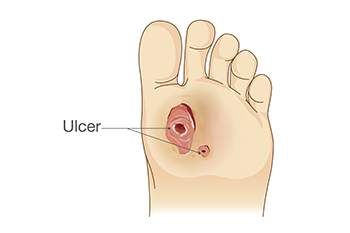
A diabetic foot ulcer is a significant and potentially serious complication arising from diabetes, characterized by open sores or wounds on the feet. The condition evolves due to a combination of factors associated with diabetes, such as impaired blood circulation, nerve damage, and compromised immune function. Elevated blood sugar levels contribute to reduced blood flow and sensation in the extremities, making the feet susceptible to injury. Minor cuts, blisters, or friction can escalate into non-healing ulcers due to the body's compromised ability to repair itself. What sets diabetic foot ulcers apart is their propensity for infection and slow healing, posing a heightened risk of severe complications if left untreated. Understanding the definition of diabetic foot ulcers underscores the importance of vigilant foot care, regular examinations, and proactive management strategies. If you have diabetes and have developed a diabetic foot ulcer, it is strongly suggested that you speak to a podiatrist who can guide you toward the best management and treatment strategies for this type of wound.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Joshua David Scoll from Pennsylvania. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Defining and Diagnosing Foot Fractures

A foot fracture, also known as a broken foot, refers to the break or crack in one or more of the bones within the foot. These fractures can result from various incidents, such as traumatic injuries, repetitive stress, or weakened bone structure. Diagnosing a foot fracture often involves a combination of physical examination and diagnostic imaging. The podiatrist will assess the injured area, looking for signs like pain, tenderness, swelling, deformity, and impaired range of motion. X-rays are the most common imaging tool used to confirm the diagnosis, allowing podiatrists to determine the type and location of the fracture accurately. Understanding the definition and diagnosis of a foot fracture is crucial for proper treatment and recovery. Whether it is a stress fracture from overuse or a traumatic injury, early diagnosis and appropriate management are essential for optimal healing and the restoration of normal foot function. If you have broken your foot, it is suggested that you consult a podiatrist who can provide one of several treatment options that are right for you.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Dr. Joshua David Scoll from Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.