
Choosing the Right Running Shoe for Your Foot Type
Running may seem like a simple to do. However, running is actually a complex movement that puts stress on the ligaments, bones, and joints of the body. Selecting the correct running shoe is important for increasing performance and avoiding risk of injury. Running shoes should be selected based on your foot type. Considerations such as trail versus road shoes are important. Your foot type dictates the degree of cushioning, stability and motion control you require. The most accurate way to learn your foot type is to visit a local shop that specializes in running shoes. Professionals can measure your arch type, stride and gait and help you with your shoe needs.
The design of running shoes is created around the idea of pronation. Pronation is the natural rolling movement of your ankle from the outside to inside when your foot strikes the ground. If you run properly you strike the ground on the outside of your heel and roll in the direction of your big toe before pushing off once more. Pronation is beneficial because it assists the lower half of your body in absorbing shock and storing energy. Those considered neutral runners pronate correctly and do not need running shoes that help correct their form. Neutral runners can choose from a wide variety of shoes, including barefoot or minimal types. However, those who have arch problems or who adopt an incorrect form while running may experience too much or too little pronation. They may require running shoes that offer additional support.
Those who overpronate experience an over-abundance of ankle rolling. Even while standing, those who severely overpronate display ankles that are angled inward. It is not uncommon for them to have flat feet or curved legs. The tendency to overpronate may cause many injuries. Areas that tend to become injured are the knees, ankles, and Achilles tendon. If you find that you have a tendency to overpronate, you should look at shoes that provide extra stability and motion-control. Motion-control shoes are straight and firm. Shoes of this type do not curve at the tip. The restricted flexibility along the middle of the shoe prohibits the foot from rolling too far inward as your foot strikes the ground.
A less common problem is underpronation. Underpronation, also called supination, is when the feet are unable to roll inward during landing. Those who underpronate have feet that lack flexibility and high arches. This prevents any kind of shock absorption, even though it does place less rotational stress on ankles and knees. This added force can cause fractures, ligament tears, and muscle strains because the legs are trying to compensate for the impact. Those who underpronate need shoes with more cushioning and flexibility. If you have a tendency to underpronate, selecting stability or motion-control shoes may cause you more problems by continuing to prevent pronation.
Treatment for Morton's Neuroma
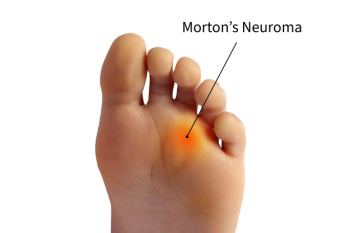 Morton’s neuroma is a painful condition that affects the ball of the foot, typically between the third and fourth toes. It involves the thickening of tissue around one of the nerves leading to the toes, often caused by irritation or compression. Symptoms include a sharp, burning pain in the ball of the foot, tingling or numbness in the toes, and the sensation of having a pebble in your shoe. A podiatrist diagnoses Morton's neuroma through a physical examination, assessing the affected area for tenderness and swelling. Imaging tests such as X-rays, ultrasound, or MRI scans may be used to rule out other conditions. The duration of symptoms can vary, with some people experiencing intermittent pain while others may have chronic discomfort. Prevention includes wearing well-fitting shoes with a wide toe box and avoiding high heels. Treatment options range from conservative approaches like rest and orthotics to corticosteroid injections and, in severe cases, surgery. For persistent pain and personalized treatment, it is suggested that you schedule an appointment with a podiatrist.
Morton’s neuroma is a painful condition that affects the ball of the foot, typically between the third and fourth toes. It involves the thickening of tissue around one of the nerves leading to the toes, often caused by irritation or compression. Symptoms include a sharp, burning pain in the ball of the foot, tingling or numbness in the toes, and the sensation of having a pebble in your shoe. A podiatrist diagnoses Morton's neuroma through a physical examination, assessing the affected area for tenderness and swelling. Imaging tests such as X-rays, ultrasound, or MRI scans may be used to rule out other conditions. The duration of symptoms can vary, with some people experiencing intermittent pain while others may have chronic discomfort. Prevention includes wearing well-fitting shoes with a wide toe box and avoiding high heels. Treatment options range from conservative approaches like rest and orthotics to corticosteroid injections and, in severe cases, surgery. For persistent pain and personalized treatment, it is suggested that you schedule an appointment with a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Joshua David Scoll of Pennsylvania. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Are Bunions Affecting Your Everyday Life?
Explaining Ulcers on the Feet

Foot ulcers, particularly common among individuals with diabetes or neuropathy, can have serious consequences if left untreated. These ulcers often start with calluses formed from repeated pressure or friction on the foot. As the skin thickens, the callus can press into the foot, killing healthy tissue and causing pain. However, neuropathy may prevent you from feeling this pain, making it harder to detect the problem early. Red, hot spots are initial signs of pressure or ill-fitting footwear. If not addressed, these can develop into blisters, corns, or calluses. Once a callus digs into the foot, it can create open wounds or ulcers, which serve as entry points for infection. Infected ulcers might discharge fluids, bleed, or emit a bad odor, and the surrounding skin may become red and warm. It's of extreme importance to address these issues promptly to prevent gangrene or limb loss. A podiatrist plays a key role in managing and preventing foot ulcers by providing specialized wound care, such as removing dead tissue. If you have developed foot ulcers, it is suggested that you make an appointment with a podiatrist for an exam and wound care options.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Joshua David Scoll from Pennsylvania. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Symptoms of Diabetic Foot Problems

Diabetes poses significant risks to foot health due to its impact on nerves, circulation, and the immune system. Peripheral neuropathy, a common complication, reduces sensation in the feet, making it difficult to detect injuries or pressure points that can lead to foot ulcers. Additionally, impaired blood flow and weakened immunity slow down healing processes, increasing the likelihood of infections that can quickly become serious. Symptoms of diabetic foot problems to watch for include persistent pain, redness, swelling, warmth, and drainage from wounds. These are potential signs of underlying issues that require immediate attention. Regular foot inspections, wearing proper footwear, and regularly scheduled appointments with a podiatrist are essential for preventing diabetic foot problems from progressing. Early intervention not only improves outcomes but also reduces the risk of complications, such as gangrene and amputation. If you have diabetes, learning how to care for your feet and recognizing the early signs of trouble are essential steps in managing your overall health. It is suggested that you add a podiatrist to your team of healthcare professionals for treating diabetes-related foot problems.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Joshua David Scoll from Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Symptoms and Diagnosis of Athlete's Foot

Athlete's foot is a common fungal infection affecting the skin on the feet, particularly between the toes. Symptoms include itching, burning, and stinging sensations, often accompanied by redness, peeling, and cracking skin. The affected areas may also appear swollen and develop blisters. Diagnosis typically involves a physical examination by a podiatrist, who may scrape a small sample of the affected skin to examine under a microscope or send it to a lab for testing. Identifying the presence of fungal elements confirms the diagnosis. Early recognition and treatment of athlete's foot are essential to relieve discomfort and prevent the infection from spreading. Proper hygiene, antifungal medications, and keeping the feet dry and clean are effective measures to manage and prevent athlete's foot. Athlete’s foot can be uncomfortable and unsightly. If you have any of the above symptoms, it is suggested that you consult a podiatrist who can successfully treat this condition, which may include prescribed medication.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Dr. Joshua David Scoll from Pennsylvania. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact one of our offices located in Philadelphia, Bensalem, and Fairless Hills, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.






